Is there a commonality between endometriosis and systemic lupus?
Aug 18, 2020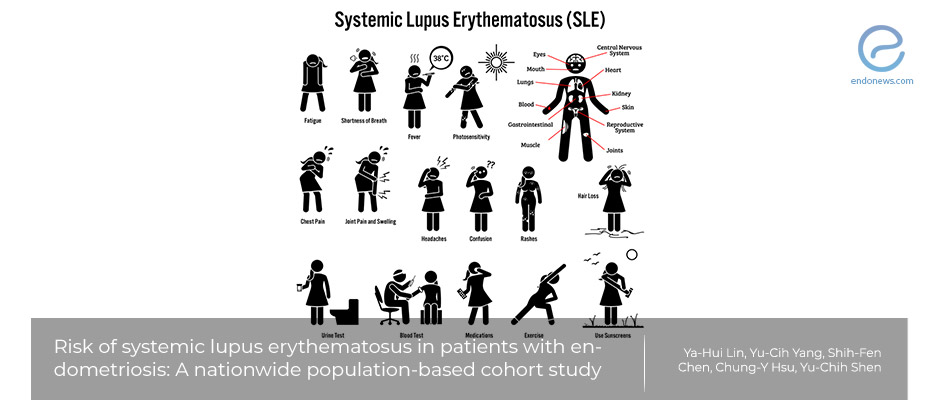
Are patients with endometriosis at increased risk of developing systemic lupus erythematosus?
Key Points
Importance:
- Are patients with endometriosis at increased risk of other pro-inflammatory and immune-dysregulation diseases such as Systemic Lupus Erythematosus (SLE)?
Highlights:
- This population-based study reveals insights into the increased risk of SLE in patients with endometriosis.
What's done here:
- This cohort study examined 17,779 patients with endometriosis and 17,779 controls (without endometriosis) matched by age, index year, and Comorbidity Index.
- The maximum follow-up period was 13 years, and the sample was representative of Taiwan.
Key Results:
- Patients with endometriosis were at increased risk of also developing SLE compared to patients without endometriosis (0.85 versus 0.57 per 1000 person-years).
- The mechanism regarding the observed increased incidence of developing SLE in patients with endometriosis is unknown, however, authors speculate that it may be due to dysregulated autoimmune responses that characterized endometriosis,
Limitations:
- This is a purely observational study and causation of the increased risk of SLE in regards to endometriosis can not be determined.
- The authors also did not study the effect of other medical co-morbidities that could have skewed their analysis between the two groups.
- This study used ultrasound for diagnosis however diagnostic laparoscopy and histologic verification is the gold standard.
Lay Summary
Systemic lupus erythematosus (SLE) is an autoimmune disease that can affect many organs including the skin, joints, the central nervous system, and the kidneys. Women of childbearing age and certain racial groups are at increased risk to develop the condition. While single-gene complement deficiencies are strongly associated with SLE, inheritance is generally is polygenic.
Genetic interactions with environmental factors, particularly UV light exposure, Epstein–Barr virus infection, and hormonal factors, might initiate the disease in those who are predisposed, resulting in immune dysregulation and a pro-inflammatory response that affects almost every organ. The diagnosis is primarily clinical and remains challenging because of the heterogeneity of SLE.
Likewise, endometriosis has been recently discerned to develop in a pro-inflammatory microenvironment and is associated with immune dysfunction. The question regarding whether endometriosis increases the likelihood of developing other autoimmune diseases is still unanswered.
A recent nationwide population-based cohort study by Lin et al. studied close to 17,800 patients in Taiwan with endometriosis and compared the incidence of SLE in patients with and without endometriosis.
Specifically, they included patients with newly diagnosed endometriosis between 1995 and 2000 and they excluded patients who were diagnosed with SLE before their initial diagnosis of endometriosis. For the control group, age-matched patients without a diagnosis of endometriosis with no prior history of SLE were included. The average follow-up year was 8.1 years for both groups.
Authors used "person-years" as an epidemiologic tool to understand the incidence of their study. A person-year measurement takes into account both the number of people in the cohort and the amount of time each person spends in the study. Thus, it can tell us the risk of a patient developing a disease in question over a long follow-up period.
The authors found that patients with endometriosis are at increased risk of developing SLE compared to patients without endometriosis. This interesting paper was published in the August 2020 issue of the "Archives of Gynecology and Obstetrics".
Research Source: https://pubmed.ncbi.nlm.nih.gov/32767040/
endometriosis inflammation surgery SLE

